Abstract
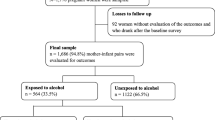
Alcohol use and HIV infection are prevalent in sub-Saharan Africa (sSA), and both are associated with low birth weight. Yet, few studies have evaluated the combined effects of maternal HIV infection and alcohol use on birth outcomes. We analyzed data from a prospective cohort study of HIV-related placental changes in Ugandan women. We defined alcohol use as self-reported alcohol use within the last year, using the AUDIT questionnaire and used linear and logistic regression to measure associations between maternal alcohol use, HIV serostatus, and birth weight. In a subsample, we measured alcohol exposure using phosphatidylethanol (PEth) in neonatal heelstick dried blood spots to confirm maternal alcohol use. Of 352 participants, 176 (50%) were women with HIV (WHIV). Three of 176 (2%) HIVuninfected women and 17/176 (10%) of WHIV self-reported alcohol use (P = 0.002). Maternal HIV infection was associated with lower birth weight (β = −0.12, 95% CI [−0.20, −0.02], P = 0.02), but self-reported alcohol use was not (β = 0.06, 95% CI [−0.15, 0.26], P = 0.54), and the interaction between HIV serostatus and alcohol use was not significant (P = 0.13). Among the PEth subsample, neither HIV status nor PEthconfirmed alcohol use were associated with low birth weight. Maternal HIV infection was associated with lower birth weight, but alcohol use was not, and there was no significant interaction between maternal HIV infection and alcohol use. Alcohol use was more prevalent in WHIV and under-reporting was common. A larger study of the effects of laboratory-confirmed alcohol and HIV exposure on birth outcomes is warranted.
Similar content being viewed by others
References
Hahn AJ, Woolf-king ES, Muyindike W. Adding fuel to the fire: Alcohol’s effect on the HIV Epidemic in Sub-Saharan Africa. Curr HIV/AIDS Rep. 2011;8(3):172–80.
Raggio AG, Psaros C, Fatch R, Goodman G, Mathews TL, Magidson FJ, et al. High rates of Biomarker-Confrimed Alcohol Use among pregnant women living with HIV in South Africa and Uganda. JAIDS J Acquir Immune Defic Syndrome. 2019;82(5):443–51.
Hahn J, Cheng D, Emenyonu N, Lloyd-Travaglini C, Fatch R, Shade S, et al. Alcohol Use and HIV Disease Progression in an antiretroviral naive cohort. J Acquir Immune Defic Syndr. 2018;77(5):492–501.
Kenya S, Chida N, Jones J, Alvarez G, Symes S, Kobetz E. Weekending in PLWH: Alcohol use and ART adherence, a pilot study. AIDS Behav. 2013;17(1):61–7.
Nachega JB, Uthman OA, Anderson J, Peltzer K, Wampold S, Cotton MF, et al. Adherence to antiretroviral therapy during and after pregnancy in low-middle and high income countries: a systematic review and meta-analysis. AIDS. 2012;26(16):2039–52.
Richardson KD, Phibbs SC, Gray EJ, McCormick CM, Workman-Daniels K, Goldman AD. Birth weight and illness severity: independent predictors of neonatal mortality. Pediatrics. 1993;91(5):969–75.
Kwang-sun L, Nigel P, Lawrence MG, Mark P. The very low-birth-weight rate: principal predictor of neonatal mortality in industrialised populations. J Pediatr. 1980;97(5):759–64.
Hack M, Klein KN, Gerry T. Long-term developmental outcomes of low birth weight infants. The Future of Children. 1995;5(1):176–96.
Peng-Lei X, Yi-Biao Z, Yue C, Mei-Xia Y, Xiu-Xia S, Yan S et al. Association between maternal HIV infection and low birth weight and prematurity: a meta-analysis of cohort studies. BMC Pregnancy Childbirth. 2015;15.
Sarah NM, Gemma AB, Lauren RD. Fetal alcohol spectrum disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin Exp Res. 2019;43(6):1046–62.
Leila G, Sarah NM. Fetal Alcohol Spectrum Disorders: a Case Study. J Pediatr Neuropsychol. 2017;3(2):114–35.
Donald AM, Fernandez A, Claborn K, Kuo C, Koen N, Zar H et al. The developmental effects of HIV and alcohol: a comparison of gestational outcomes among babies from south african communities with high prevalence of HIV and alcohol use. AIDS Res Ther. 2017;14(28).
Bajunirwe F, Haberer EJ, Boum IIY, Hunt P, Mocelo R, Martin NJ, et al. Comparison of self-reported alcohol consumption to Phosphatidylethanol Measurement among HIV-Infected patients initiating antiretroviral treatment in Southwestern Uganda. PLoS ONE. 2014;9(12):e113152.
Asiimwe SB, Fatch R, Emenyonu NI, Muyindike WR, Kekibiina A, Santos GM et al. Comparison of Traditional and Novel Self-Report Measures to an Alcohol Biomarker for Quantifying Alcohol Consumption Among HIV-Infected Adults in Sub-Saharan Africa. Alcoholism: Clinical and Experimental Research. 2015;39(8):1518–27.
Bebell ML, Siedner JM, Ngonzi J, Le HM, Adong J, Boatin AA, et al. Brief report: chronic placental inflammation among women living with HIV in Uganda. JAIDS J Acquir Immune Defic Syndrome. 2020;85(3):320–4.
Harris AP, Taylor R, Thielke R, Jonathan P, Gonzalez N, Conde GJ. Research electronic data capture(REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
WHO. Alcohol Use Disorders Identification Test. 2001.
Polcin LD, Galloway PG, Bond J, Korcha R, Greenfield KT. Confirmatory factor analysis and test-retest reliability of the Alcohol and Drug Confrontational Scale (ADCS). J Drug Issues. 2009;39(4):931–48.
Jones J, Jones M, Plate C, Lewis D. The detection of 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoethanol in human dried blood spots. Anal Methods. 2011;3(5):1101–6.
Hahn JA, Dobkin LM, Mayanja B, Emenyonu NI, Isaac M, Shiboski S, et al. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV positives in sub-saharan Africa. Alcohol Clin Exp Res. 2012;36(5):854–62.
Stewart SH, Koch DG, Willner IR, Anton RF, Reuben A. Validation of Blood Phosphatidylethanol as an Alcohol Consumption Biomarker in Patients with Chronic Liver Disease. Alcoholism: Clinical and Experimental Research. 2014;38(6):1706–11.
Baldwin AE, Hayes N, Ostrander E, Magri R, Sass N, Mesquita M dos. Phosphatidylethanol (PEth) levels in post-partum women and their newborns in Uruguay and Brazil. Alcohol Clin Exp Res. 2020;44(6):1292–9.
W.H.O. Global Nutrition targets 2025: Low Birth weight Policy Brief.
Twabi S, Manda O, Small S. Assessing the effects of maternal HIV infection on pregnancy outcomes usng cross-sectional data in Malawi. BMC Public Health. 2020;20.
van der Merwe K, Hoffman R, Black V, Chersich M, Coovadia A, Rees H. Birth outcomes in south african women receiving highly active antiretroviral therapy: a retrospective observaional study. J Int AIDS Soc. 2011;14.
Kumar B, Handelman K, Voronkin I, Mwapasa V, Janies D, Rogerson J et al. Different regions of HIV-1 subtype C env are associated with placental localization and in utero mother-to child transmission. Am Soc Microbiol Journals. 2011;85(14).
Moussa M, Roques P, Fievet N, Menu E, Maldonado-Estrada J, Brunerie J, et al. Placental cytokine and chemokine production in HIV-1-infected women: trophoblast cells show a different pattern compared to cells from HIV negative women. Clin Exp Immunol. 2001;125(3):455–64.
Krishna U, Bhalerao S. Placenta insufficincy and fetal growth restriction. J Obstet Gynaecol India. 2011;61(5):505–11.
Dreyfuss L, Msamanga I, Spiegelman D, Hunter J, Urassa J, Hertzmark E, et al. Determinants of low birth weight among HIV-infected pregnant women in Tanzania. Am J Clin Nutr. 2001;74(6):814–26.
Lundsberg S, Illuzi L, Belanger K, Triche W, Bracken B. Low to moderate prenatal alcohol consumption and the risk of selected birth outcomes: a prospective study. Ann Epidemiol. 2015;25(1):46–54e3.
Lundsberg S, Bracken B, Saftlas F. Low-to-moderate gestational alcohol use and intrauterine growth retardation, low birth weight and preterm delivery. Ann Epidemiol. 1997;7(7):498–508.
Mills L, Graubard I, Harley E, Rhoads G, Berendes W. Maternal alcohol consumption and birth weight. How much drinking during pregnany is safe? JAMA. 1984;252(14):1875–9.
Nykjaer C, Alwan AN, Greenwood CD, Simpson A, Hay, White L et al. Maternal alcohol intake prior and during pregnancy and risk of adverse birth outcomes: evidence from a british cohort. BMJ J Epidemiol Community Health. 2013;68(6).
Adong J, Fatch R, Emenyonu N, Cheng D, Muyindike W, Ngabirano C, et al. Social desirability bias impacts self-reported alcohol use among persons with HIV in Uganda. Alcohol Clin Exp Res. 2019;43(12):2591–8.
Funding
This work was supported by the Harvard University Center for AIDS Research National Institutes of Health/National Institute of Allergy and Infectious Diseases [grant number P30AI060354 to LMB] and supported by a KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst | The Harvard Clinical and Translational Science Center [grant number KL2TR002542 to LMB], and the Charles H. Hood Foundation (to LMB), a career development award from the National Institute of Allergy and Infectious Diseases [grant number K23AI138856 to LMB], midcareer mentoring awards [grant number K24AI141036 to IVB, K24AA022586 to JAH, K24 HL166024 to MJS], the Weissman Family MGH Research Scholar Award (to IVB), and the American Society of Tropical Medicine and Hygiene Burroughs Wellcome Postdoctoral Fellowship in Tropical Infectious Diseases (to LMB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The sponsors had no role in study design, data collection, analysis or interpretation, writing the report, or decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, the National Institutes of Health, or other funders.
Conflict of Interest
None of the authors have a commercial or other association that might pose a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Adong, J., Musinguzi, N., Ngonzi, J. et al. Effects of Maternal HIV Infection and Alcohol Use in Pregnancy on Birth Outcomes in Uganda. AIDS Behav 28, 805–810 (2024). https://doi.org/10.1007/s10461-023-04181-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04181-2