Abstract
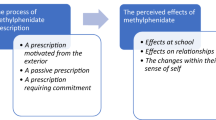
Fetal Alcohol Spectrum Disorders (FASD) refer to physical, cognitive, and behavioural symptoms in an individual whose mother consumed alcohol during pregnancy. It is the leading cause of non-genetic avoidable mental disability, with an estimated worldwide prevalence of 1%. Attention Deficit Hyperactivity Disorder (ADHD) diagnostic criteria are met for 50–80% of patients with FASD. Methylphenidate (MPH) is the first-line pharmacological treatment for ADHD. This study aims to explore the lived experience of children with FASD taking MPH and their caregivers to adapt prescribing modalities by considering different ways to administer the drugs. We hope to improve the therapeutic alliance between the children and their caregivers by gaining an insiders’ view of the medication perception. Semi-structured interviews with children and their caregivers were conducted in this qualitative study. Data collection by purposive sampling continued until we reached theoretical sufficiency. Data were analysed using interpretative phenomenological analysis. We conducted 16 semi-structured interviews: 8 with the children aged 7–12, 5 boys and 3 girls and 8 with their caregivers. The analysis showed that inadequate palatability and capsule form experiences were the leading causes of children's non-adherence to the treatment. MPH appeared to be a valuable aid for caregivers even if they had concerns about its potential toxicity. However, it is necessary to identify caregivers' expectations concerning MPH to adapt the prescription in terms of choice of specialty and intake modalities. Regular support was required to reduce caregivers’ fears of dependence, personality transformation and long-term adverse effects. Information on palatability should be given when prescribing MPH to children with ADHD as well as its possible side effects or toxicity. It highlights the need for further studies of the experience of palatability of drugs prescribed to children. When prescribing a treatment, children should be more involved in medical counselling and it is necessary to understand the child's perspectives to co-construct common representations for better therapeutical adherence.




Similar content being viewed by others
Availability of data and material
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- CG:
-
Caregiver
- FAS:
-
Fetal alcohol syndrome
- FASD:
-
Fetal alcohol spectrum disorder
- FP:
-
Foster parents
- IPA:
-
Interpretive phenomenological analysis
- MPH:
-
Methylphenidate
- PIP:
-
Paediatric investigation plans
- WISC-5:
-
Wechsler intelligence scale for children - 5th edition
- YCESS-RS:
-
Young child emotional state self-rating scale
References
Haute Autorité de Santé (HAS) (2013) Troubles causés par l’alcoolisation fœtale : repérage
Ministère du travail de l’emploi et de la santé (2011) Alcool et grossesse, parlons-en. Guide à l’usage des professionnels. Paris
Le syndrome d’alcoolisme foetal (2002) Paediatr Child Health 7:181–95
Nordmann R (2004) Consommation d’alcool, de tabac ou de cannabis au cours de la grossesse. Académie nationale de médecine | Une institution dans son temps 519–21
Dörrie N, Föcker M, Freunscht I, Hebebrand J (2014) Fetal alcohol spectrum disorders. Eur Child Adolesc Psychiatry 23:863–875. https://doi.org/10.1007/s00787-014-0571-6
Astley SJ (2010) Profile of the first 1,400 patients receiving diagnostic evaluations for fetal alcohol spectrum disorder at the Washington State Fetal Alcohol Syndrome Diagnostic & Prevention Network. Can J Clin Pharmacol 17:e132-164
Santé publique France (2018) Baromètre santé 2017. Alcool et tabac. Consommation d’alcool et de tabac pendant la grossesse
Furtado EF, de Roriz ST (2016) Inattention and impulsivity associated with prenatal alcohol exposure in a prospective cohort study with 11-years-old Brazilian children. Eur Child Adolesc Psychiatry 25:1327–1335. https://doi.org/10.1007/s00787-016-0857-y
Mick E, Biederman J, Faraone SV, Sayer J, Kleinman S (2002) Case-control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. J Am Acad Child Adolesc Psychiatry 41:378–385. https://doi.org/10.1097/00004583-200204000-00009
(1999) A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal treatment study of children with ADHD. Arch Gen Psychiatry 56:1073–86. https://doi.org/10.1001/archpsyc.56.12.1073.
Ritfeld GJ, Kable JA, Holton JE, Coles CD (2022) Psychopharmacological treatments in children with fetal alcohol spectrum disorders: a review. Child Psychiatry Hum Dev 53:268–277. https://doi.org/10.1007/s10578-021-01124-7
Peadon E, Rhys-Jones B, Bower C, Elliott EJ (2009) Systematic review of interventions for children with fetal alcohol spectrum disorders. BMC Pediatr 9:35. https://doi.org/10.1186/1471-2431-9-35
Snyder J, Nanson J, Snyder R, Block GJ, Nanson J, Snyder R, Block G (1997) A study of stimulant medication in children with FAS. In: Overcoming and preventing secondary disabilities in fetal alcohol syndrome and fetal alcohol effects, 64–77
Oesterheld JR, Kofoed L, Tervo R, Fogas B, Wilson A, Fiechtner H (1998) Effectiveness of methylphenidate in native American children with fetal alcohol syndrome and attention deficit/hyperactivity disorder: a controlled pilot study. J Child Adolesc Psychopharmacol 8:39–48. https://doi.org/10.1089/cap.1998.8.39
Doig J, McLennan JD, Gibbard WB (2008) Medication effects on symptoms of attention-deficit/hyperactivity disorder in children with fetal alcohol spectrum disorder. J Child Adolesc Psychopharmacol 18:365–371. https://doi.org/10.1089/cap.2007.0121
Rowles BM, Findling RL (2010) Review of pharmacotherapy options for the treatment of attention-deficit/hyperactivity disorder (ADHD) and ADHD-like symptoms in children and adolescents with developmental disorders. Dev Disabil Res Revs 16:273–282. https://doi.org/10.1002/ddrr.120
Coe J, Sidders J, Riley K, Waltermire J, Hagerman RJ (2001) A survey of medication responses in children and adolescents with fetal alcohol syndrome. Mental Health Aspects Dev Disabil 4:148–155
Ghosh M, Fisher C, Preen DB, Holman CDJ (2016) “It has to be fixed”: a qualitative inquiry into perceived ADHD behaviour among affected individuals and parents in Western Australia. BMC Health Serv Res 16:141. https://doi.org/10.1186/s12913-016-1399-1
King J, Brosseau L, Guitard P, Laroche C, Barette JA, Cardinal D et al (2019) Validation transculturelle de contenu de la version franco-canadienne de l’échelle COREQ. Physiother Can 71:222–230. https://doi.org/10.3138/ptc.2018-44.f
Mays N, Pope C (2000) Qualitative research in health care. Assessing quality in qualitative research. BMJ 320:50–52. https://doi.org/10.1136/bmj.320.7226.50
Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B et al (2018) Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 52:1893–1907. https://doi.org/10.1007/s11135-017-0574-8
Largy P (2018) De l’auto-évaluation de l’état émotionnel du jeune enfant : l’échelle AEJE, 461–9
Boyer A, Noël R (2018) Les parents funambules : entre désir d’enfant et désir d’accueil, un équilibre à négocier dans la famille d’accueil régulière au Québec
Smith J, Flowers P, Larkin M (2009) Interpretative phenomenological analysis: theory, method and research 6
Antoine P, Smith JA (2017) Saisir l’expérience : présentation de l’analyse phénoménologique interprétative comme méthodologie qualitative en psychologie. Psychol Fr 62:373–385. https://doi.org/10.1016/j.psfr.2016.04.001
Alexandre B, Reynaud E, Osiurak F, Navarro J (2018) Acceptance and acceptability criteria: a literature review. Cogn Technol Work 20(2):165–177. https://doi.org/10.1007/s10111-018-0459-1
Cram A, Breitkreutz J, Desset-Brèthes S, Nunn T, Tuleu C, European Paediatric Formulation Initiative (EuPFI) (2009) Challenges of developing palatable oral paediatric formulations. Int J Pharm 365:1–3. https://doi.org/10.1016/j.ijpharm.2008.09.015
Standing J, Tuleu C (2005) Paediatric formulations—getting to the heart of the problem. Int J Pharm 300:56–66. https://doi.org/10.1016/j.ijpharm.2005.05.006
Nunn T, Williams J (2005) Formulation of medicines for children. Br J Clin Pharmacol 59:674–676. https://doi.org/10.1111/j.1365-2125.2005.02410.x
Akrich M (1996) Le médicament comme objet technique. Revue internationale de Psychopathologie, 135
Caliman L, Prado-Martin MR (2019) Prise de psychostimulants et attention : l’expérience de deux adolescents diagnostiqués TDAH au Brésil et en France. La Nouvelle Revue Education et Societe Inclusives 85:261–276
Ahmed R, McCaffery KJ, Aslani P (2013) Factors influencing parental decision making about stimulant treatment for attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 23:163–178. https://doi.org/10.1089/cap.2012.0087
Hansen DL, Hansen EH (2006) Caught in a balancing act: parents’ dilemmas regarding their ADHD child’s treatment with stimulant medication. Qual Health Res 16:1267–1285. https://doi.org/10.1177/1049732306292543
Chapon-Crouzet N (2018) Les différents modes de suppléance en famille d’accueil. Quelles relations entre l’enfant confié, ses parents et sa famille d’accueil? Revue des Politiques Sociales et Familiales 128:7–21. https://doi.org/10.3406/caf.2018.3299
Chapon N (2014) Parentalité d’accueil et relations affectives. Presses universitaires de Provence, Aix En Provence
Bernard A, Sanahuja A (2019) L’enfant « corps-étranger-familier » en famille d’accueil. Le Divan Familial 42:163. https://doi.org/10.3917/difa.042.0163
McDougall S, Finlay-Jones A, Arney F, Gordon A (2020) A qualitative examination of the cognitive and behavioural challenges experienced by children with fetal alcohol spectrum disorder. Res Dev Disabil 104:103683. https://doi.org/10.1016/j.ridd.2020.103683
Welniarz B, Medjdoub H (2018) Resumen. L’information psychiatrique 94:460–467
Coletti DJ, Pappadopulos E, Katsiotas NJ, Berest A, Jensen PS, Kafantaris V (2012) Parent perspectives on the decision to initiate medication treatment of attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 22:226–237. https://doi.org/10.1089/cap.2011.0090
Benkert O, Graf-Morgenstern M, Hillert A, Sandmann J, Ehmig SC, Weissbecker H et al (1997) Public opinion on psychotropic drugs: an analysis of the factors influencing acceptance or rejection. J Nerv Ment Dis 185:151–158. https://doi.org/10.1097/00005053-199703000-00004
Falissard B (2014) Les médicaments de l’attention : les doutes d’un praticien. Esprit 34–43
Taylor M, O’Donoghue T, Houghton S (2006) To medicate or not to medicate? the decision-making process of Western Australian parents following their child’s diagnosis with an attention deficit hyperactivity disorder. Int J Disabil Dev Educ 53:111–128. https://doi.org/10.1080/10349120500510115
Brinkman WB, Sherman SN, Zmitrovich AR, Visscher MO, Crosby LE, Phelan KJ et al (2009) Parental angst making and revisiting decisions about treatment of attention-deficit/hyperactivity disorder. Pediatrics 124:580–589. https://doi.org/10.1542/peds.2008-2569
Leslie LK, Plemmons D, Monn AR, Palinkas LA (2007) Investigating ADHD treatment trajectories: listening to families’ stories about medication use. J Dev Behav Pediatr 28:179–188. https://doi.org/10.1097/DBP.0b013e3180324d9a
Acknowledgements
We would like to thank the participants of this study, and Pr Patricia Dobkin for the English proofreading.
Funding
We would like to thank the French Congress of Psychiatry for funding this project.
Author information
Authors and Affiliations
Contributions
MS and BD conceived the design and methodology; CM conducted the research interviews, CM, MS, CD, JB, NB performed the data analysis. CM wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests or potential conflicts to disclose.
Ethics approval and consent to participate
An authorization was obtained from the French Commission Nationale de l'Informatique et des Libertés (2206739 v 0). All participants provided oral informed consent before inclusion.
Consent for publication
All participants gave their consent.
Ethics approval
An authorization was obtained from the French Commission Nationale de l'Informatique et des Libertés (2206739 v 0).
Consent to participate
All children and their parents provided written consent before inclusion in the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morin, C., Doray, B., Dumar, C. et al. Qualitative study of the lived experience of methylphenidate prescribed for children with a fetal alcohol spectrum disorder. Eur Child Adolesc Psychiatry 33, 4219–4235 (2024). https://doi.org/10.1007/s00787-024-02457-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-024-02457-z